
Health Minister Rachel Stephen-Smith would not say whether the ACT’s high golden staph infection rates represented a systemic issue. Photo: Thomas Lucraft.
ACT Health Minister Rachel Stephen-Smith has admitted rates of golden staph infection in the Territory’s public hospitals are trending in the “wrong direction”.
Golden staph (also known as Staphylococcus aureus) is a common and usually harmless type of bacterium that lives on people’s skin and in their noses; however, it can cause potentially life-threatening infections if it enters a person’s bloodstream through a skin cut. This is known as a Staphylococcus aureus bloodstream infection, or golden staph infection.
Shadow Health Minister Leanne Castley seized on the ACT’s public hospitals recording the highest rate of these infections in the latest reporting period.
“This is another nation-lagging low for Canberra’s public health system under the Barr-Rattenbury Government,” she said.
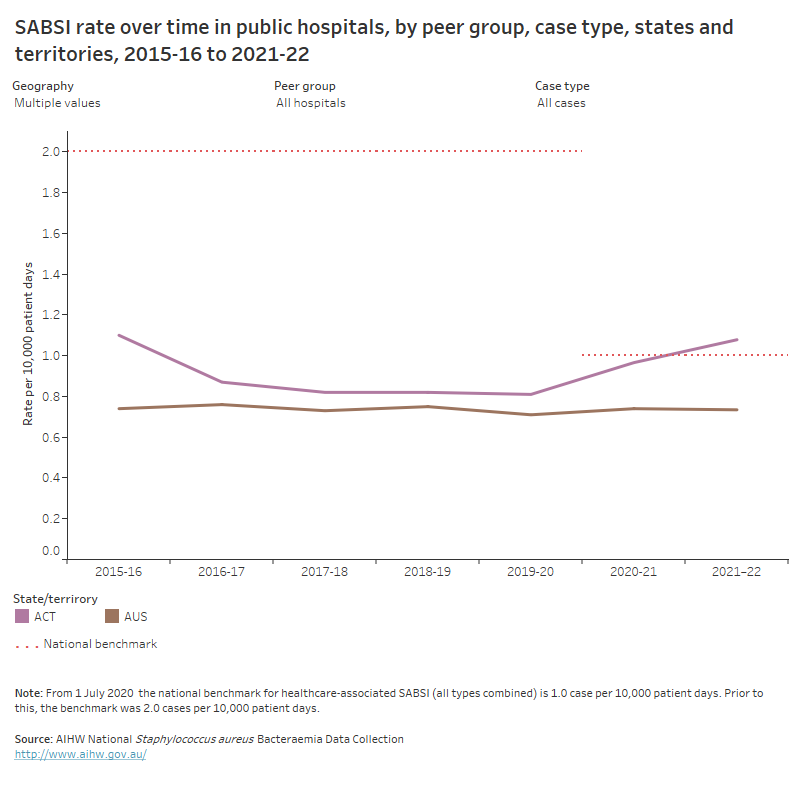
Golden staph infections in ACT public hospitals increased between the two most recent reporting periods. Photo: AIHW.
Data for 2022-23 has not been released and the estimated rate of infections for the period was listed as “N/A” in the recent ACT Budget papers.
Ms Castley said the ACT’s Digital Health Record reporting was “a fiasco” and it was incomprehensible the figures could not be provided, even manually.
In the most recently released data, the ACT’s public hospitals recorded 45 golden staph infections at a rate of 1.08 per 10,000 patient days.
The Canberra Hospital was the worst-performing public hospital in the ACT, recording the majority of the ACT’s cases (35), at a rate of 1.26 infections per 10,000 patient days.
While the ACT has consistently recorded one of the lowest overall numbers of infections in the country, it has registered the highest rate of infections for the past two reporting periods.
The 2021-22 rate in ACT’s public hospitals exceeded the national figure (0.73) and it was the only state or territory to exceed the national benchmark infection rate (1.0).
However, a CHS spokesperson said comparing the ACT and Canberra Hospital to other states and territories was “not advised” because the ACT lacked smaller regional hospitals, which generally provided more routine health care, and its larger hospitals, namely Canberra Hospital, provided complex medical care that may be more susceptible to instances of golden staph infections.
“In addition, when data from different jurisdictions is compared, jurisdictions may vary in admission practices, patient case mix and surveillance methodology,” the spokesperson said.
“The best way for Canberra Hospital to compare is directly with own past performance, and CHS has been trending down since 2020-21.”
While under questioning by Ms Castley, Minister Stephen-Smith made a similar argument about drawing comparisons, but reached a different conclusion.
“Our trend has been going in the wrong direction and that’s why there has been extra effort going into ensuring that comes back down,” she said.
Under further questioning, she added: “Overall, we need to bring that [findings] together and understand if there is a systemic concern.”
Ms Stephen-Smith’s office was approached for comment. It referred Region to the statement provided by the CHS spokesperson.
While the overall rate of infections in ACT’s public hospitals increased between 2020-21 and 2021-22, the rates decreased between these two periods at both CHS-run hospitals.
The only public hospital to record an infection rate increase between these periods was the then-Calvary-run public hospital in Bruce, though it still outperformed Canberra Hospital.
A CHS spokesperson said while their performance improved in the period before Bruce Hospital became a CHS asset, they aimed to continue to improve “over and above the peer benchmark”.
“There are a range of actions we take when a case of [golden staph] infection is notified, not only to manage the individual occurrence but to reduce instances occurring in the future,” the spokesperson said.
The spokesperson said these actions included reviewing hand-hygiene compliance and processes related to contact with body fluids and tissue, providing specialised infection prevention and control input and support, conducting a comprehensive audit on cannula (a thin tube inserted into a vein or other body cavity) management, and additional education and training for staff.
Outside of these actions triggered by identified golden staph infections, the spokesperson said, CHS also conducted screening tests before operations and ensured sterile contact with patients’ skin.
“Antimicrobial stewardship is also a key cornerstone of reducing the rates of antibiotic resistance,” the spokesperson said. “This means making sure patients receive the right antibiotics, at the right time.”
Of the 45 golden staph infections reported in ACT public hospitals, most (42) were treatable with commonly used antibiotics and only three were resistant.


















