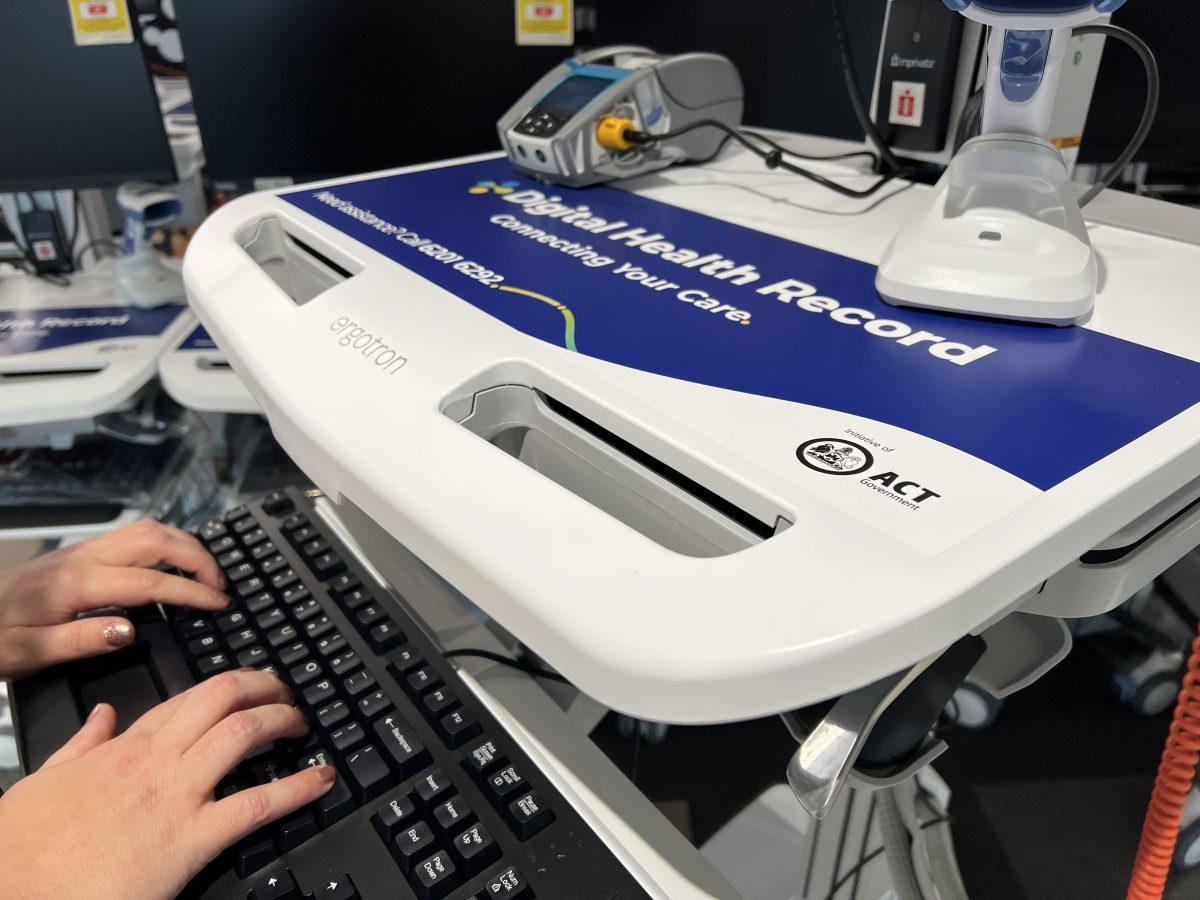
The Digital Health Record system will go live in exactly three months across the Territory’s public health system. Photo: Lottie Twyford.
In exactly three months’ time, a single patient records system will be rolled out across the Territory’s public health system.
When it does, it will replace a mishmash of more than 40 existing systems.
The move to the Digital Health Record is touted by the government to make life easier for patients and clinicians, although some challenges and additional work for staff are anticipated in the first instance.
What is the Digital Health Record?
Essentially, it’s a Territory-wide records system that will be used at public hospitals, walk-in centres, community health centres and justice health services.
It will also have a patient-facing application that healthcare consumers can download and use.

ACT Health chief information officer Peter O’Halloran and chief nursing and midwifery information officer Rebecca Heland are counting down the days until ‘go live’. Photo: Lottie Twyford.
What are the benefits?
Because information will be stored in one place, clinicians and healthcare staff can find it more quickly and easily.
Detailed data will include who administered medication and at what time, as well as information from devices such as heart rate monitors. It should mean treating clinicians are able to spend more time with their patients.
Preparation is underway to ensure any IT issues in those early days from Monday, 14 November can be dealt with promptly.
Isn’t this just a Federal Government thing?
No. That’s the My Health Record.
Essentially, the Digital Health Record is much more detailed and contains information inputted to use in real-time by healthcare staff.
My Health Record is really just a summary.
“Imagine it like this,” ACT Health chief information officer Peter O’Halloran said. “If you’re admitted to hospital as an in-patient for a week, that might generate between 200 to 400 pages of information about you. [The hospital] provides about six to eight of those to My Health Record.
“What we are rolling out will do everything from work out who is in each bed, who is next on the elective surgery list and what allergies you have. My Health Record will just show a patient went to hospital and had a procedure.”
Haven’t I used this before?
Quite possibly.
ACT Health chief nursing and midwifery information officer Rebecca Heland said people might already remember the MyDHR app from the days of booking in for their COVID-19 vaccinations.
“That same app is about to undergo a really significant upgrade so patients who see any clinician or specialist across the healthcare system will be able to see information about upcoming appointments, after-visit summary notes, letters, pathology and imaging results,” she said.
Already, 187,000 people have downloaded the MyDHR app.
What does this new system mean for patients?
Patients will be able to access more information about their own care.
The app can also be used to help save time as patients who need surgery in hospital can read through information about their procedure and be ready to ask questions once they turn up.
But according to Mr O’Halloran, the big change on day one will be for staff.
Are healthcare staff happy about the change?
Some healthcare staff have previously raised concerns about the timing to implement the new system given the ongoing health pressures due to the pandemic and high rates of winter illnesses.
But Ms Heland said staff would be extensively supported and trained in the lead-up to November, and once the system went live.
She said 14,500 users needed to be trained in the new system and 8000 devices would need to be rolled out across 45 locations before the implementation date.
She also stressed international experience had shown the system would make life easier for staff after only a couple of weeks.
“The current situation can be complicated for nurses across all specialities because patients often have information stored across different areas,” she said.
“It will be a learning curve – that’s for sure.”
Can I opt out?
No.
Health information for the app is already being collected via IT and hard copy.
You can choose whether you want your GP or the private system to access your record.
Do you need to be IT savvy?
Patients need a bit of know-how to use the app and need a smartphone.
But Mr O’Halloran stressed the app wasn’t mandatory; clinicians would still use the system on their end.
ACT Health is working alongside the Healthcare Consumers Association to help ensure cohorts less comfortable with technology can reap the benefits.




















