
The AMA says the integration of North Canberra Hospital into CHS presents an opportunity to better coordinate the Territory’s public hospital services. Photo: Claire Fenwicke.
State and territory health ministers have been presented with some sobering reading by the Australian Medical Association (AMA) on the state of public hospital surgery wait times in Australia, with the AMA claiming the system is at “breaking point”.
The ACT health system had mixed results in the report card, with the AMA saying ACT public hospitals are performing below the standard the community should expect.
For emergency department wait times, the ACT sits on the median of all states and territories, midway between the best and worst-performing states, but is the worst-performing jurisdiction for patients being seen and completed within four hours.
“The ACT continues to struggle under the ‘four-hour rule’, with only 48 per cent of emergency department presentations being completed in less than the requisite four hours,” ACT AMA president Dr Walter Abhayaratna said.
“This result has been in decline for almost a decade now. ACT residents deserve better. While it’s little comfort to know that public hospital performance is down across the country, it does show just how much pressure all our public hospitals are under.”
In its annual Public Hospital Report Card, the AMA says planned surgery wait times in public hospitals are the longest they’ve ever been, and has called on all health ministers to take urgent action to relieve pressure on the system.
The report card uses data from the Australian Institute of Health and Welfare to present a snapshot of Australia’s public hospital performance.
AMA president Professor Steve Robson said it clearly demonstrated the need for urgent action on top of existing planned changes to the National Health Reform Agreement (NHRA), and that he had written to all health ministers ahead of their planned meeting today requesting an additional $4.12 billion investment in an urgent national plan.
“After a decade of declining performance, health ministers late last year agreed to a new funding model for public hospitals that will see the Commonwealth increase its share of the funding and change the cap on funding growth,” Professor Robson said.
“This announcement followed tireless AMA advocacy for funding reform, but it doesn’t come into effect until 2025. Unfortunately, this year’s report card shows that our hospitals are at breaking point.
“Urgent action is needed now.”
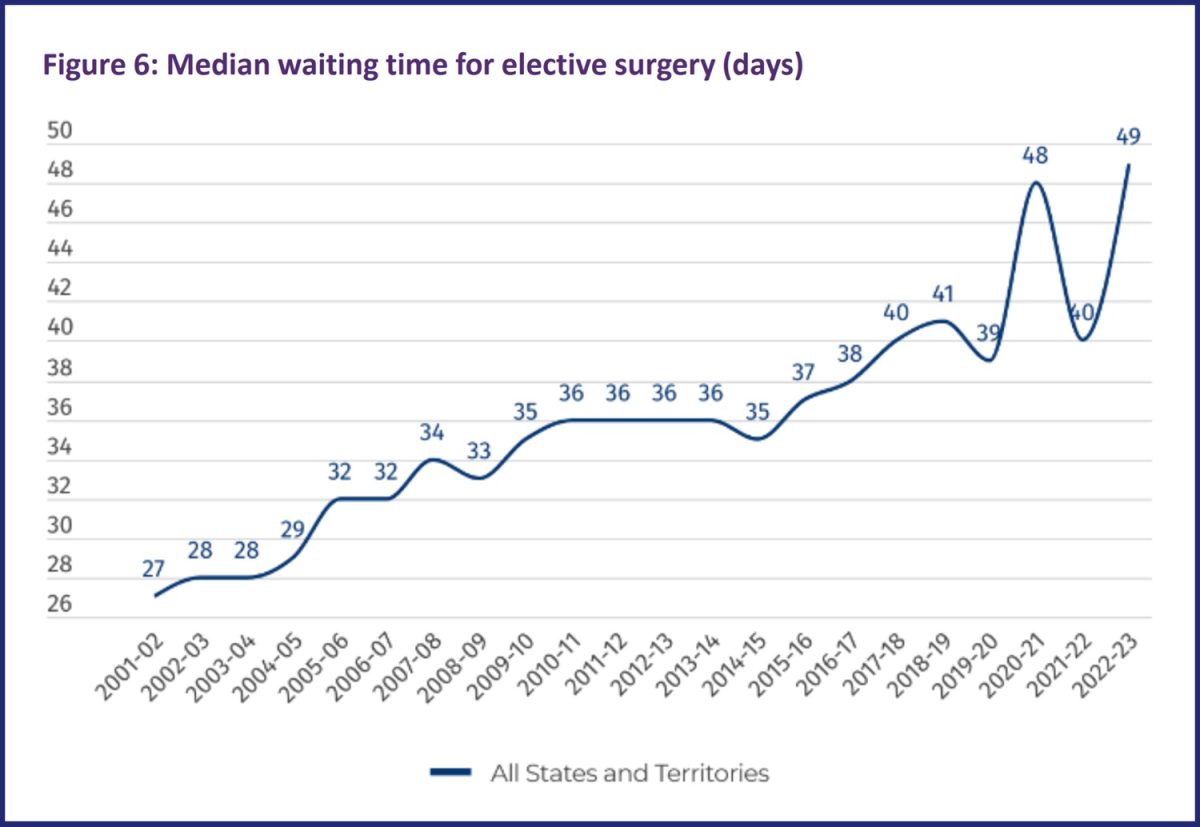
The median elective surgery wait time of 49 days is now one day worse than at the height of the COVID-19 pandemic. Image: AMA.
The AMA defines planned surgery as any form of surgery considered medically necessary, but which can be delayed at least 24 hours.
It says the median wait time for planned surgery indicates the number of days within which 50 per cent of patients were admitted for their planned procedure. This means half of the patients had a shorter wait time than the median, and half had a longer wait time.
For 2022-23, that median increased by nine days to 49, one higher than the previous worst year, 2020-21, during the height of the COVID-19 pandemic, 13 days longer than 2012-13, and 21 days longer than 2002-03.
It also highlighted that population growth has outpaced the number of hospital beds available. In the four years to 2021-22, Australia’s population grew by more than a million, but only 1200 hospital beds were added. This decreased Australia’s public hospital capacity from 2.53 beds to 2.47 beds per 1000 people.
ACT Shadow Minister for Health and Deputy Opposition Leader Leanne Castley said it was unacceptable for only 47 per cent of emergency visits in the ACT to be completed within the four hours.
“This is the lowest level of patients being seen within four hours in the ACT for the fifth year in a row and it is clear that the ministers’ solutions to address these issues are simply not working,” she said.
“If the minister continues to ignore primary health care in the ACT then Canberrans will continue to present to our emergency departments, which puts further pressure on the hospital system along with the hardworking doctors and nurses.”
Ms Castley said the report card also indicated that the ACT had the worst record for the number of planned surgery patients admitted on time.
“Elective surgery and outpatient waitlists have continued to decline despite the government promising Canberrans to restore these waitlists so that they meet clinically recommended timeframes,” she said.
Dr Abhayaratna said the integration of North Canberra Hospital into Canberra Health Services presented an opportunity to better coordinate the Territory’s public hospital services, and that more streamlined services would be the result. He also hoped that, with 2024 being an election year, a vigorous and policy-driven debate about the ACT’s local healthcare system would take place.
“The lead-up to this year’s election will also see the opening of the Canberra Hospital expansion, with all the excitement and challenges that go with it,” he said.
“It’s to be hoped that the new facility will provide a much-needed boost to our hard-working staff and play an important role as the ACT seeks to turn around its public hospital performance.
“But one thing we do know is that a decade of walk-in centres has not improved the ACT’s public hospital emergency waiting times, and change is needed.
“Disappointingly, the ACT Government does not seem to appreciate that the continued funding of fragmented care, and the imposition of a payroll tax on medical practices, will result in increased utilisation of emergency departments as the cost of care in the community for those with chronic diseases increases.
“In turn, this will result in more pressure on our hospitals, and an increase in high-cost, hospital-based care that should have been provided earlier and at a lower cost in the community.”




















