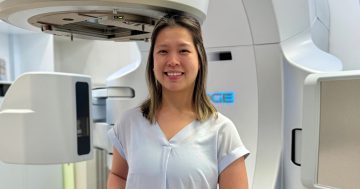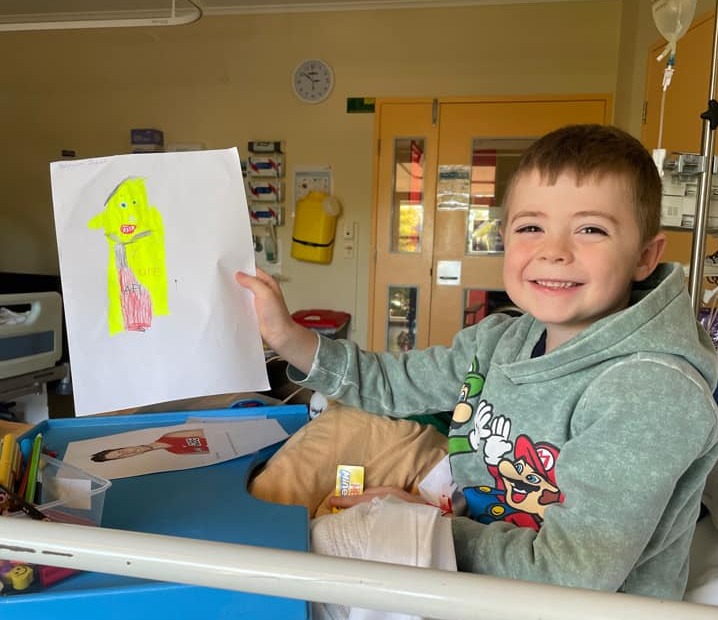
William will likely spend six months in hospital in Sydney receiving treatment. Photo: Alisha Konig.
Unable to work, unable to go to school, unable to stay at their home – and all with an extremely sick and in-pain young child to care for – that’s the reality for this young family.
Exhausted mum Alisha Konig is renewing calls for both the ACT and Federal Governments to commit to establishing paediatric oncology services in the capital.
Her eight-year-old son William is currently receiving care for relapsed stage three neuroblastoma at The Children’s Hospital at Westmead in Sydney.
That means Alisha, her husband Scott Phillips and their other three children have packed up their lives, left their jobs and been pulled out of school to live in Ronald McDonald House while William receives his second lot of treatment.
What’s worse is that the family has no idea how long this will continue.
“It’s really hard. Scott has gone on leave without pay from his job because he needs to care for the other children while I’m in the hospital with William,” she explains.
“So, we’re also all effectively separated at all times.”

The family pictured all together (before the most recent arrival). Photo: Supplied.
William was first diagnosed with cancer in 2020. The first time, he spent eight months in hospital in Sydney.
That period was complicated by the pandemic, of course, and travel restrictions between NSW and the ACT at various times, and they’ve been back in Sydney since William’s relapse was confirmed in May this year.
“We’ve been given a tentative figure of six months, but that’s assuming everything goes well – and we know with cancer that things don’t tend to go to plan,” Alisha explains.
Obviously, life is difficult for William – who is now in Year 1 at Namadgi School. He is in a lot of pain, and Alisha says he is finding it difficult to go through treatment again.
The family has also been warned to prepare themselves for future relapses and that William’s chances of a full recovery are slim.
But the impact on his two older siblings is also immense, as well as the new baby the family welcomed last year.
“No school or daycare and no structure means they are going back in terms of learning and also behaviour,” Alisha notes.
Like many families in this situation, Alisa has turned to crowd-funding to help with some of the expenses.
But with potentially years of this ahead of her, Alisha notes the worries about the children, her finances and her marriage are kicking in.
“I’ve even had discussions with my husband about what’s going to happen to our super because, at the moment, we’re not getting any – so it’s going to have these disastrous effects for years and years even after all of this is well and truly over,” she says.
Her mental health is also suffering.
“You basically never stop. You never get to check out and you never get a break. You just have to adapt this nurse-like mentality where you stop being a mum and you start being a caretaker,” Alisha explains.
“Even if you have a supportive network, which I do, it’s a lot.”
Not having to travel to Sydney to access care for William wouldn’t change all of this, of course, but it would alleviate some of the pressure which comes from being taken away from that network.
She’s asked before why Canberra can’t have specialist paediatric oncology services of its own. The responses she usually gets are along the lines of there not being enough specialists who are willing to come and work in Canberra.
Alisha finds this argument difficult to accept given that many of the families she has met in Sydney are also travelling from Canberra or the surrounding region.
“It’s not just us! I find it strange that [the government] doesn’t believe there’s a need for paediatric oncology,” she says.
Minister for Health Rachel Stephen-Smith said there is currently insufficient demand in the ACT to sustain a safe paediatric oncology service delivering quality care.
“The Government often faces a tension when planning for specialised, low-volume health services. In some cases, it makes sense to plan for additional investment and capacity for the ACT as the local population and demand grow over time,” she said.
“However, in other cases, there isn’t enough volume for the local service to build up enough expertise and capability, and agreements are developed to ensure care for ACT residents in a more established service.
“I understand that it is extremely difficult for families facing the dual challenge of a very sick child and the need to travel for care. We are committed to doing more to support these families, which is why we commissioned the Health Care Consumers’ Association to undertake the Kids Interstate Shared Care Project in 2019-20 to identify opportunities to improve care for these families.”
A spokesperson for Federal Health Minister Mark Butler said the provision of oncology services in Canberra is a matter for the ACT Government.