Overdoses and hepatitis C infection continue to be a deadly problem. Photo: File.
Another step has been taken towards finally establishing a safe injecting facility for illicit drug users after ACT Health contracted the Melbourne-based Macfarlane Burnett Institute for Medical and Public health to conduct a feasibility study.
ACT Health expects a draft report to be submitted by 30 June and a final report by 14 August.
The ACT Drug Strategy Action Plan, launched in December 2018, put the controversial idea of a medically supervised place where illicit drug users could inject safely to avoid possible overdose and prevent hepatitis C infection back on the agenda after multiple failures to set up a trial since the 1990s.
In 1997, the then Prime Minister John Howard sparked a territory rights row when he intervened to stop a six-month trial. But sentiment has shifted in recent years towards harm minimisation and treating drug addiction as a health issue.
When launching the Action Plan in 2018, former ACT health minister Meegan Fitzharris said the injecting room prioritised screening, testing, treatment and harm reduction with evidence-based responses to drug use.
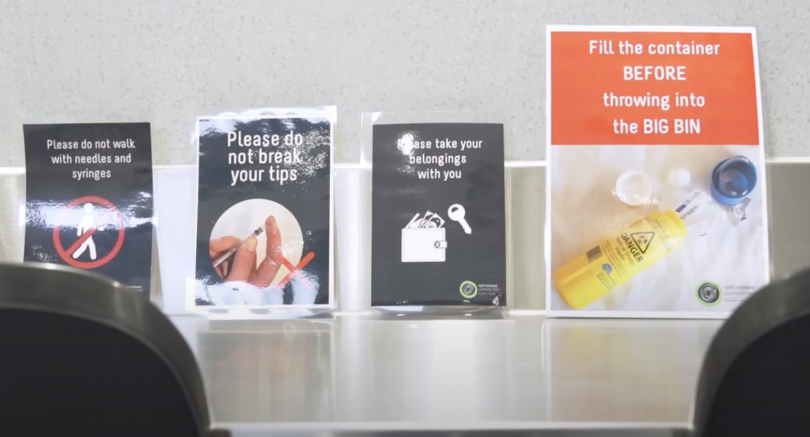
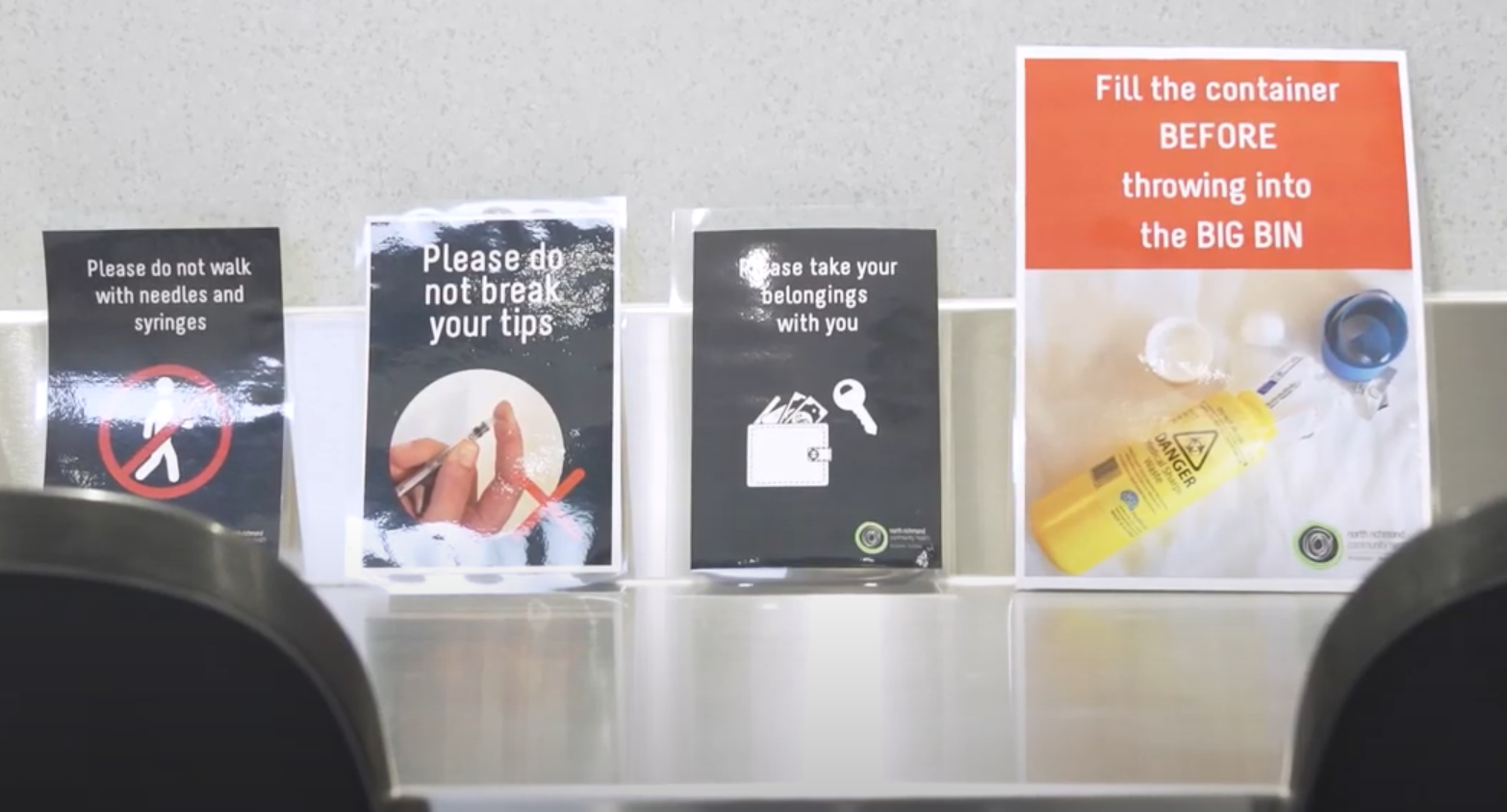
Advice at the North Richmond safe injecting facility. Photo: Victoria Government.
“Every year there are over 1000 admissions to our hospitals from overdoses,” she said.
“We know that the effects of drug use can be devastating, not only for those who use drugs, but also for their friends and family and the broader community.”
She said the government was committed to increasing treatment options, noting the increasing use and misuse of opioids, both illicit and prescription.
“It’s also concerning to see opioid deaths on the rise. That’s why we will look to explore the feasibility and need for a medically supervised injecting room here in Canberra, which is something that has been established in other cities already.”
Part of the brief for the Macfarlane Burnett Institute will be to review models used in Australia and internationally, including the longstanding injecting room in Sydney and the current two-year trial in North Richmond in Melbourne.
It will have to assess the need for such a service in Canberra, identifying current and future patterns of drug use patterns, risk behaviours, and drug-related health problems.
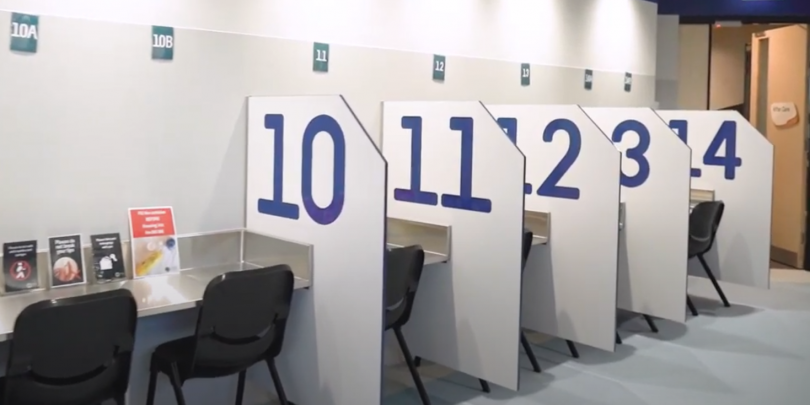
Cubicles at the North Richmond facility. Photo: Victoria Government.
It should also consider whether any service should be able to check or test drugs being used for impurities and dangerous substances and/or provide needles and syringes.
This is in line with the government’s support for pill testing at events such as music festivals, and possibly a permanent site for testing.
If the Institute recommends that the ACT establish an injecting room, it should advise on an appropriate model for the service and whether it should be stand-alone or integrated with primary care and/or other services, or if it should be a fixed site or a mobile facility.
It should also list any support services that could be part of a service, and which substances and methods of administering drugs it should focus on.
ACT Health also wants to know how much such a service would cost to set up and operate, as well as how many staff would be needed.
Program Director Behaviours and Health Risks Professor Paul Dietze will lead the project.
The contract is worth $207,680.